Opening Times | Contact Us | Patient Access
CQC Rating Good
Open letter to our patients of Len Valley Practice
We are aware that there are at times difficulties accessing care and advice at Len Valley Practice.
We are aware of the negative comments about primary care in general, both in the media and the local social media
We thought we could help our patients understand why we are so busy at the surgery, and this is not isolated to us, it is a national problem.
There are lots of reasons why we are seeing huge increases in demand. Some of these are to do with Covid-19, such as:
- Backlog of work built up during lockdowns
- Now an increase in seasonal viruses following lockdowns
- Another wave of Covid-19, despite the effectiveness of the vaccinations limiting the most serious effects of the virus, and the media silence on this despite Covid-19 is still present and on the rise. This has a knock on effect on staff sickness and absence as the healthcare profession are still hampered by the social isolation rules
- Increased waiting lists for hospital appointments and planned surgery meaning some people are living with untreated conditions and need ongoing and increasingly complex support from the General Practice team. Hospital teams are under similar pressures to GPs.
There are also pressures that existed before the pandemic, for example:
- GP workload has grown in volume, complexity and intensity. It is taking longer to provide safe effective clinical care of our patients.
- Recruiting into General practice teams. Recruitment and retention are huge issues within primary care teams and this is also effecting us at the surgery. There is a lot of bad press about GPs and their teams in the media as well as social media, it has a massive impact on the resilience of the team.
- Infrastructure and premises. Having taken back control of our Harrietsham Branch Surgery back from our Primary Care Network (PCN)- following the vaccination roll out - there are awful unresolved IT issues causing the computer system to not function at a level that would allow us to work within the surgery at present. These are being dealt with via BT. We hope to return to usual service when this is resolved and our staffing situation allows.
Contrary to reporting by the media, Len Valley Practice have been open throughout the pandemic and, although the way we work had to change to protect our patients, we have they never stopped seeing people.
Why is it more difficult to see a member of the general practice team face-to-face?
- Face-to-face appointments have been back at pre-pandemic levels consistently since around June 2021 with some short-term exceptions.
- Between April 2019 and February 2020 (10 months prior to the pandemic), general practice in Kent and Medway carried out 7.5million appointments.
- Between April 2021 and February 2022 (10 months ‘post’-pandemic), Kent and Medway practices delivered over 9million total appointments.
- General practice carried out over 1.5million more appointments in the same time period.
- The number of face-to-face appointments has remained around the same at just over 5million a year. This means that while a lower percentage of total appointments are taking place face-to-face, the same number of face to face appointments are being carried out. Were these to increase the number of appointments offered would need to be reduced.
- These national figures are certainly reflected in our work at the surgery here.
How are practices working?
Most practices had started to introduce telephone triage before the pandemic and, although circumstances sped up adoption in some areas, this is now how most practices will work in the future, and how we are working at Len Valley at present.
Appointment requests and other queries are triaged by a trained call handler to identify the right member of staff to see the patient through the right type of appointment.
The Doctors are able to deal with many issues over the phone that do not require a face to face appointment. This allows us to deal with more patients than returning to the traditional 10 mins booked appointments. When we feel a face to face appointment is required, we are able to be flexible about meeting these needs on the day or another day.
You may visit the surgery and at times it would appear as if nobody is in waiting room to see the Doctor. Please be assured that we are in our rooms dealing with the influx of calls each day.
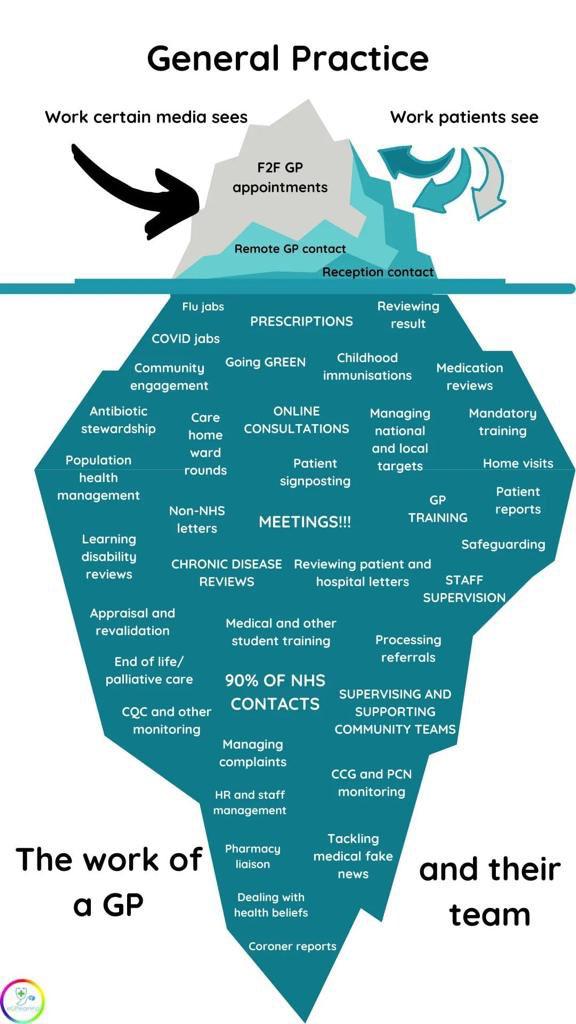
However, there is only so much that we can do in a work day at the surgery. We are already working over and above the recommended BMA suggested workload each day, and there is other work that is required to be on the day as well as trying to meet the needs of our patients. Administrative workload has spiralled and a lot of time removes us from being able to perform our clinical roles. Below show some of the other hidden roles that are not recognised:
We are considering using an online triage system for those people who have digital access to be able to request an appointment without needing to call the practice. This is being piloting within our PCN (in other practices) currently.
We have been extremely fortunate to have recruited 2 new partners following Dr Hagan and Dr Taylor leaving partnership, at a time when other surgeries have been unable to recruitment and in cases having to close completely.
We are also in a slightly better position than others in securing 2 new salaried Doctors who are able to start (August and September) which will help alleviate the immense stress we are under. We are still understaffed and have positions to fill though, but there is not a pool of Doctors out there.
Before the last election the Conservatives pledges 6000 more GPs by 2024, yet this will not happen. The number of full time GPs has fallen by 29,263 in 2015 to 27,627 in May 2022. Newer qualified GPs do not work to work full time due to the immense pressures and senior GPs are stepping down to reduce their work load.
The multi-professional team
The workforce in General Practice has been changing for some time with a range of trained clinicians now working in practices, making sure patients can see the right person, first time. These include paramedics, nurse practitioners and social prescribers. More information on these roles can be found here.
When you call the practice you will be asked questions to determine who is best for you to see, which may not always be a GP. It is important to give as much information to the highly skilled receptionist to make this process effective.
Other actions include:
- Hospital waiting list queries – people on hospital waiting lists have traditionally had to contact their general practice for updates, which needs the practice to follow up with the hospital. We are working with all hospitals to implement direct enquiries services to make it easier for patients, and try to direct patient to the hospital teams for information
- medication on discharge – people leaving hospital often need continuing medication, but were routinely prescribed just two to three days of supply by the hospital, meaning people have to quickly contact their practice to arrange further supplies. We are hoping this will be tackled in the near future to avoid people having to go back to their GP so quickly. The same occurs for Medical Certificates.
- Internal hospital referrals – if one hospital service sees a patient and identifies a need for an appointment with another service, the patient is normally directed back to general practice to make a new referral. This is just wasted administrative time for all involved a delay in patients care and we are trying to tackle on a daily basis with hopeful improvements eventually.
- Promoting alternative services – 111, pharmacies and urgent treatment centres can provide the advice and care that some patients need. When are appointments are full on the day, the receptionist are asked by the Doctors to suggest that patients consider these routes for further advice if they are unable to secure a telephone triage appointment on that day.
- Phone system capabilities – having recently introduced a new phone system that was all singing and dancing, it is proving inadequate for the level of demand now being experienced. We have secured some funding to improve this shortly.
Pressure on general practice is also related to workforce and infrastructure challenges (such as buildings or systems), which existed before the pandemic and need longer-term solutions.
Whilst trying to repair Harrietsham, we are also at the tail end of applying for an extension at Len Valley Practice which has been in the planning stage for the last 3 years and delayed due to the Covid Pandemic. As well as more clinical rooms, we are increasing the size of our dispensary, with our main aim to make our dispensing more efficient for our patients.
We hope this goes someway to explaining the challenges within Primary care at the moment and in your Surgery.
Please remember that as GPs, we have gone into practice to care for our patients. We are on the frontline of the NHS managing a dire situation. We are your advocate and we share your frustrations when you face difficulties accessing help and advice through the surgery and long waiting times for routine appointments. We want better services too. Please understand we are all just trying to do the very best we can to provide much needed care in a depleted system with inadequate resources available to us. We are all hopeful that things will improve at some time.
Dr Andrew Reed
Len Valley Practice
On behalf of Drs Kendrew, Welsh, Lloyd and West.
Published: Aug 4, 2022
We use cookies to help provide you with the best possible online experience.
By using this site, you agree that we may store and access cookies on your device. Cookie policy.
Cookie settings.
Functional Cookies
Functional Cookies are enabled by default at all times so that we can save your preferences for cookie settings and ensure site works and delivers best experience.
3rd Party Cookies
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
